An Economist's View to Healthcare
HAIs are very common today and represent a significant impact to society.
According to a 2019 CBS poll,1 for about 43% of Americans, affording medical care is a financial hardship. While the reasons for high health care costs is varied and nuanced, the occurrence and treatment of health care associated infections, typically known as HAIs, is a factor in the problem. HAIs not only contribute to the high costs for patients, but they are also significantly more costly for healthcare facilities and providers.
The CDC states2 that HAIs, "cost billions of dollars in added expenses to the healthcare system," between S97-147 billion annually,3 to be precise.

Unfortunately, HAIs are very common. In fact, the CDC estimates,2 "that on any given day, 1 in 31 hospital patients has an HAI," which is about 3% of all patients. HAIs can stem from a number of different problems; everything from human error to unprecedented pandemics. As a result, many facilities feel overwhelmed by the prospect and potential cost associated with preventing HAIs. Ignoring HAIs is not going to solve the problem or save a facility money. There are enormous costs that could come from disregarding preventative measures to avoid spreading HAIs to unsuspecting patients. Fortunately, there are various low-cost solutions that can be a part of a facility's risk mitigation strategy when it comes to infection prevention.
HAIs are such a rampant problem in health care that The Joint Commission (TJC) identified the reduction of HAIs as one of their top five National Patient Safety Goals4 for 2020. They are not the only ones; even the U.S. Department of Health and Human Services (HHS)5 has identified the reduction of HAIs as an Agency Priority Goal. Decreasing instances of HAIs must be the goal of every health care facility with a view to keep their own costs down and, more importantly, to keep providers' promises to patients to do them no harm. To effectively tackle the HAI problem, one must identify the most common causes of HAIs which can be addressed.

Premier Safety Institute6 explains that patients are, "at increased risk of HAIs from exposure to organisms that are transmitted between bpatients and healthcare workers." So, in essence, one of the most common causes of HAIs can be traced back to basic human error. When looking specifically at the reprocessing of ultrasound probes, like transesophageal echocardiogram (TEE) ultrasound probes, there are some points in the process that are especially vulnerable to human error.
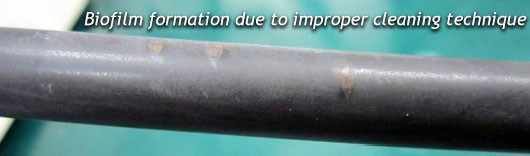
To begin with, merely handling long, delicate TEE probes can prove cumbersome and lead to a probe being damaged. Damage to the probe's shaft can lead to nicks and abrasions which harbor bacteria and encourage the development of nearly impossible to clean biofilm. This sort of damage requires very costly repairs which cannot be put off; biofilm on a probe's shaft presents a huge liability and puts patients at an increased risk of contracting an HAI.

Probes can also be significantly damaged during the cleaning and disinfecting process when these steps are carried out manually. Moving a probe from basin to basin is likely to result in a few bumps and dings which could affect the ultra-sensitive distal tip, which is incredibly costly to fix. Additionally, the probe handle is liable to slip into a tub of cleaner or disinfectant which in many cases will render the probe unusable and may require a total replacement of the ultrasound probe.
According to David Dallaire, the Director of Sales of Acertara Labs7 which specializes in probe repair, "TEE repairs range from about $1,800 to $9,000 with an average of $4,250." So for each case of damage to a probe, a facility is facing, on average, about a $4,000 bill. The more TEE ultrasound probes are manually handled, the higher the chances of needing more repairs throughout the year.

Human error can also present itself in the form of stressed out, overworked, and hurried staff members. Especially with the turn of events in recent months due to COVID-19/SARS-CoV-2, healthcare facilities are faced with a high volume of patients, increased rules, and stricter policies, but with no increase of help. As a result, many healthcare workers are at the end of their ropes. In this condition, it is easy to lose track of which steps have been completed in the long string of steps required to properly reprocess TEE probes. It is also easy to be pulled in so many directions that steps are skipped and time is not kept track of when manually reprocessing
When manually reprocessing probes, there are so many things that can go wrong at every turn if all factors are not attended to perfectly. The temperature of the cleaning solution and later of the high-level disinfectant (HLD) must be closely monitored and kept within a particular range. If not, there is the risk that the probe will not ultimately be high-level disinfected. When dealing with overworked and stressed staff, it is possible for the cleaning step to be skipped altogether, which is a major oversight which can lead to the buildup of bacteria and the formation of biofilm. If a TEE probe is not fully dried after disinfection, the risk of bacterial growth increases significantly. And if a probe is not stored in a way that prevents recontamination, the probe is also at risk of harboring harmful bacteria. If any of these steps goes wrong because of an honest mistake or oversight, a patient's health and even life could be put in jeopardy.
While there is an inestimable human cost to the transmission of an HAI to a patient, there are also tangible, financial consequences to the spread of an HAI. The National Institutes of Health (NIH)8 note that HAIs are, "associated with increased resource consumption (more blood tests, imaging, antibiotic days, hospital days, etc).
11 When investigating the cost of managing care for an HAI, the Agency for Healthcare Research and Quality (AHRQ),9 "found the average cost attributable on a per-case basis to be approximately 531,000. The least expensive infectious HAI is CAUTI (513,793), and the most expensive is CLABSI (S48, 108)."
Another example can be seen in Clostridium Difficile, one of the most common causes of HAIs in the US, which increases a patient's hospital stay by 2.8-5.5 days, according to The Society for Healthcare Epidemiology of America (SHEA).10 Each one of those days racks up thousands of dollars in expenses; according to Debt. org,11 in 2017, "Hospital costs averaged $3,949 per day and each hospital stay cost an average of $15,734."

These costs are very high when one considers that they apply to 3% of all patients to enter a healthcare facility. Consequently, in an effort to reduce costs and encourage hospitals to improve quality, the Centers for Medicare and Medicaid Services (CMS), "has stopped paying for select 'preventable complications', some of which are HAls."12 So the brunt of this added cost may fall on the already burdened shoulders of health care facilities or, worse, on the heads of the unfortunate patients who were infected.
The high costs of transmitting an HAI to a patient do not stop there; there are more factors to take into consideration. Transmission of an HAI may lead to a medical malpractice lawsuit for a facility and/or its providers. Legal fees, lawsuits, and settlements related to infecting a patient can cost a facility millions of dollars. Becker's Hospital Review13 reports that, "The typical hospital is the target of seven HAI-related lawsuits per year with an average settlement of $1.5 million, for a total of $10.5 million per hospital. Now that 27 states require hospitals to report incidence of HAIs, the number of awards is expected to rise."

Lastly, there are reputational costs for a facility that is associated with the spread of HAIs. A Pew Research14 poll indicated that, "44% of internet users look online for information about doctors or other health professionals." That means that nearly half of all patients are going to be in the know in regards to their local health care facilities. If there are negative reviews or local news stories about HAIs or other outbreaks, prospective patients are sure to know. As reported by Becker's Hospital Review,15 a survey by PricewaterhouseCoopers on healthcare and social media showed that a whopping 41% of consumers say social media affects their hospital choice.
If a hospital or health care facility develops a negative reputation online and in the community, that will certainly make its way to their bottom line. The truth is there is no way of really pinning down an exact number of what this could cost a facility, but we do know the consequences could be dire. A bad reputation definitely means a loss of revenue and may even go as far as endangering the future prospects of a facility. That alone should be encouragement enough to spur health care facilities to do whatever possible to reduce the spread of HAIs.

Looking at the incredibly high costs that could be incurred by a facility for just one HAI, it is critical that health care institutions take the time to minimize this risk.
One of the most effective tools in the arsenal for fighting HAIs is automation. According to the Health Service Executive16 of Ireland, "Internationally it is recognised [sic] that the use of an automated validated process for decontaminating RIMD will provide enhanced risk reduction of infection transmission." When reprocessed by an FDA-cleared automated system, ultrasound probes are considerably more likely to be reprocessed correctly. Scientifically validated automated reprocessors will ensure the time, temperature, and amount of chemical being used is correct each time. According to The Society of Diagnostic Medical Sonography (SDMS),17 "Automated processes are preferable due to the reduced risk of operator error." By simply automating the processes of cleaning and high-level disinfecting TEE probes, one can mitigate a significant amount of the risk posed by the possibility of human error.
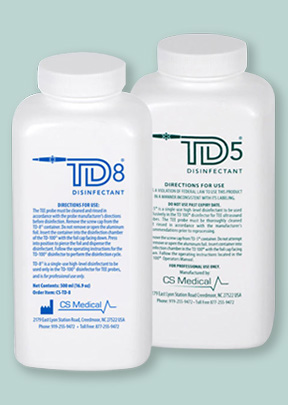
Single-use HLDs are another tool that can be utilized to minimize the risk of HAIs. When reprocessing ultrasound probes, infection preventionists (IPs) or reprocessing technicians need to measure the potency of reusable disinfectants before each use. This opens the door for mistakes and for misreadings of sometimes complex test strips. If, instead, only single-use HLDs are used, then the chances of using an ineffective HLD are greatly diminished. This helps ensure that probes are reprocessed with H LDs that are potent enough to neutralize any harmful bacteria each and every time.
One more way for hospitals and facilities to keep patients safe from HAIs with regards to TEE probes in particular is to make sure all relevant staff is appropriately trained in infection prevention and each step of the reprocessing procedure. Ensuring each staff member is regularly trained in reprocessing probes and in using any automated reprocessors will reduce the chances that they will miss or skip steps due to ignorance or lack of understanding the importance of each step. Additionally, facilities may want to consider the value of web-based training as they try to comply with social distancing guidelines and the new risks posed by COVI D-19/SARS CoV-2. Making sure staff is properly trained is not only good form, it is also required for accreditation by TJC. Standard LD.01.03.01 states:18 "Initial and on-going competency, training, and adhering to manufacturer's instructions for use and evidence-based guidelines are important to patient safety."

With all the financial pitfalls facing health care institutions, it is worth investing a significant amount of time and money into preventing the possibility of the spread of HAIs. Health care professionals invest so much time and put so much of their hearts into caring for patients. Allowing the transmission of an HAI to annihilate all that work would be short sighted and unwise. While the upfront expense of implementing automation, single-use HLDs, and comprehensive staff training may be daunting, they more than pay for themselves in short order. These changes should not be considered costs, but should be understood as investments in the future of a facility and, by extension, investments in the community. Attending to the financial wellbeing of a facility is not just good for the bottom line of the institution, it is good for the patients and local community being served. The benefits of implementing these strategies far outweigh the cost of new equipment.
References:
1. https://drive.google.com/file/d/0ByVu4fDHYJgVTUZwcEM4TmJNRE1IQXlfTWFCZXlreWNZQkdv/view
2. https://www.cdc.gov/hai/eip/antibiotic-use.html
3.
https://www.researchgate.net/publication/256499741_Economic_Burden_of_Healthcare-Associated_Infection_in_US_Acute_Care_Hospitals_-_Societal_Perspective
4.
https://www.jointcommission.org/-/media/tjc/documents/standards/national-patient-safety-goals/2020/2020-hap-npsg-goals-final.pdf?db=web&hash=17AB9546CAD521158182BC25A8387B2E
5. https://health.gov/our-work/health-care-quality/health-care-associated-infections
6.
https://www.premiersafetyinstitute.org/safety-topics-az/healthcare-associated-infections-HAIs/hai/
7. https://www.acertaralabs.com/
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7358996/
9. https://www.ahrq.gov/hai/pfp/haccost2017-results.html
10. https://www.guidelinecentral.com/share/pocketcard/53d67314007df/#i31631411
11. https://www.debt.org/medical/hospital-surgery-costs/
12. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2827870/
13.
https://www.beckershospitalreview.com/quality/hospital-acquired-infections-by-the-numbers.html
14. https://www.pewresearch.org/internet/2011/02/01/health-topics-3/
15.
https://www.beckershospitalreview.com/hospital-management-administration/41-of-consumers-say-social-media-affects-their-hospital-choice.html
16.
https://www.hse.ie/eng/about/who/qid/nationalsafetyprogrammes/decontamination/ultrasound-probe-decontamination-guidance-feb-17.pdf
17.
https://www.sdms.org/docs/default-source/Resources/2018-sdms-ic-guidelines-and-appendices---draft-2-public-comments.pdf?status=Temp&sfvrsn=0.8523093232394274
18.
https://www.jointcommission.org/-/media/enterprise/tjc/tjc-documents/to-delete-documents/private-for-hidden-content/tjc_hld_boosterpakpdf.pdf?db=web&hash=5805EEA1131DAB35E767E906F1AODF15