Improved Patient Care with a HAI Reduction Solution
Introduction
The Centers for Disease Control and Prevention (CDC) estimates that three percent of all patients treated in medical facilities contract infections; these are called healthcare associated infections, or HAis. These HAis not only harm individuals, but the hospitals themselves. Becker's Hospital Review reports that, "The total direct, indirect and nonmedical social costs of HAis are estimated at around $96 billion to $147 billion annually."
Reusable medical devices are a contributing factor to these statistics. These devices must be reprocessed between each patient to prevent the spread of disease caused by microorganisms. If they are not properly reprocessed every single time they are used, the chances of spreading an HAI increase. Adherence to rigorous reprocessing protocols for semi-critical medical devices is imperative for any healthcare infection prevention strategy and for promoting patient safety.
One element of that protocol which is often underrated is the cleaning step. While achieving high-level disinfection is largely dependent upon having a quality disinfectant and optimal disinfection conditions, the importance of cleaning in the disinfection process must not be overlooked.
The importance of cleaning
Cleaning is the process of removing debris or foreign materials from medical devices (CDC, 2008). During procedures, endocavity and ultrasound probes can come in contact with multiple patient tissues, resulting in contamination of probes with soil and microorganisms. Even when probes are used with sheaths, they may be covered in gels or the sheath can sometimes become compromised during the procedure unbeknownst to the operator. Cleaning helps to remove these soils and begin to break down the bioburden left behind in order to properly disinfect these devices.
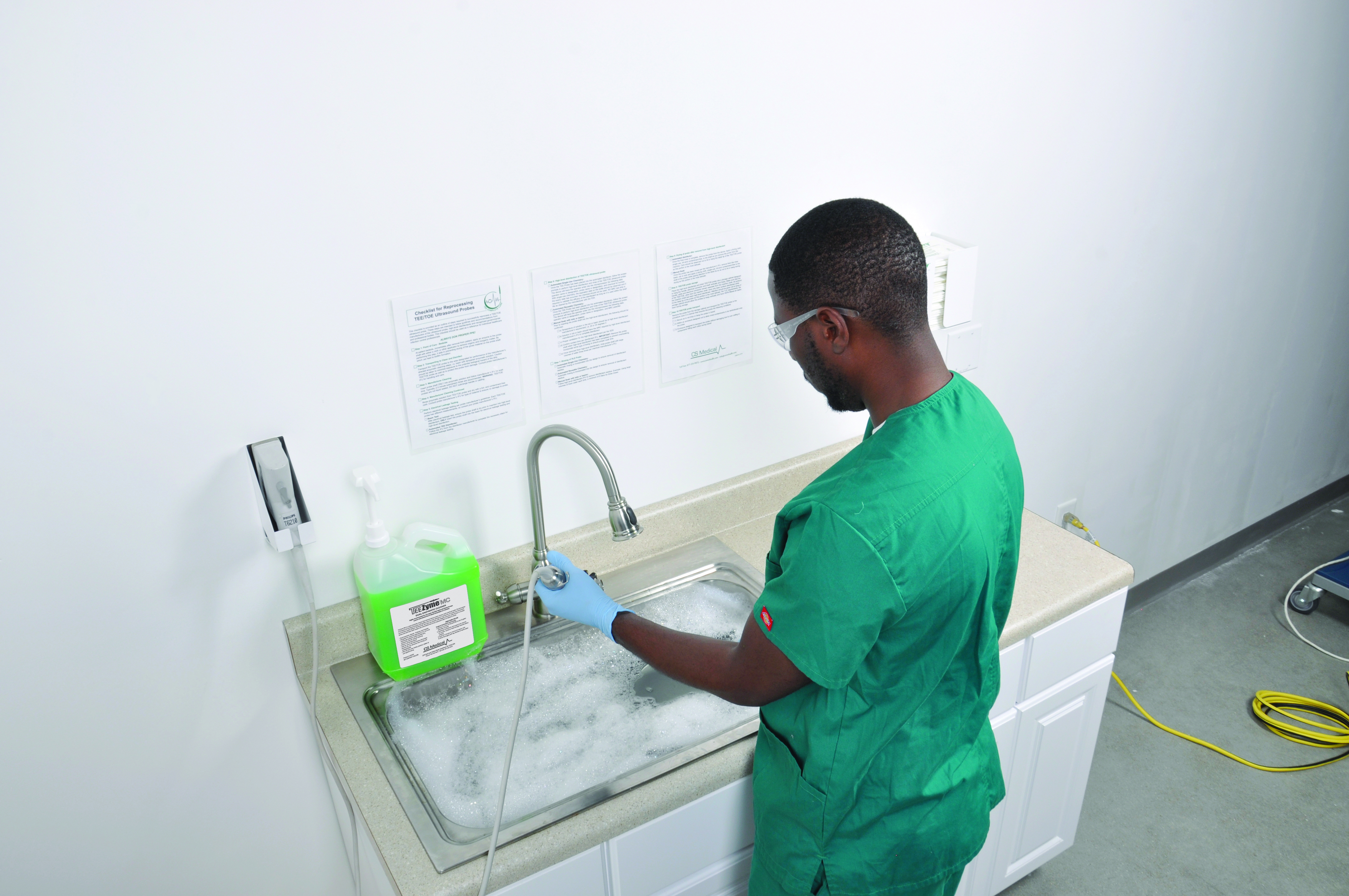
Manual cleaning requires space and dedication to following instructions each and every instance.
The cleaning process is essential to achieve high-level disinfection. Cleaning alone can help reduce the numbers of microorganisms from reusable medical devices by 4-6 logl O (CDC, 2008). Microorganisms on probes can be Reusable medical devices are a contributing factor to these statistics. These devices must be reprocessed between each patient to prevent the spread of disease caused by microorganisms. If they are not properly reprocessed every single time they are used, the chances of spreading an HAI increase. Adherence to rigorous reprocessing protocols for semi-critical medical devices is imperative for any healthcare infection prevention strategy and for promoting patient safety. One element of that protocol which is often underrated is the cleaning step. While achieving high-level disinfection is largely dependent upon having a quality disinfectant and optimal disinfection conditions, the importance of cleaning in the disinfection process must not be overlooked. Cleaning is the process of removing debris or foreign materials from medical devices (CDC, 2008). During procedures, endocavity and ultrasound probes can come in contact with multiple patient tissues, resulting in contamination of probes with soil and microorganisms. Even when probes are used with sheaths, they may be covered in gels or the sheath can sometimes become compromised during the procedure unbeknownst to the operator. Cleaning helps to remove these soils and begin to break down the bioburden left behind in order to properly disinfect these devices. The cleaning process is essential to achieve high-level disinfection. Cleaning alone can help reduce the numbers of microorganisms from reusable medical devices by 4-6 logl O (CDC, 2008). Microorganisms on probes can be more difficult to kill when they are present in high numbers (CDC, 2008). Inadequate cleaning will leave higher numbers of organisms on the device, perhaps even more than can be removed by disinfection alone, putting the next patient's health in jeopardy (Rutala, 2014). Debris on reusable medical devices can also directly lead to improper disinfection. Debris can physically block contact of the disinfectant with the device's surface (CDC, 2008, Lewis 1995, Muscarella 1995). Further, soil or debris components can inhibit or inactivate the active ingredients in some disinfectants (Lambert, 2001, Rutala 1997) and simply make high-level disinfectants less effective overall.
Over time, if probes are not properly cleaned and disinfected after every use, the remaining debris and ineffective disinfection will promote the formation of microbial biofilms (Alfa, 2009, Roberts, 2013). Biofilms are a protective layer or matrix which encloses and preserves communities of microorganisms (Donlan, 2002). Once a microorganism is contained in biofilm, it is much more difficult or even impossible to remove and kill, even when the correct cleaning and disinfection procedures are followed (Alfa, 2009). The greatest defense against biofilms is proper cleaning and disinfection of devices after each use to prevent biofilm formation altogether.
Effects of improper cleaning
Biofilm formation due to improper cleaning technique.

Typical setup for reprocessing using the basin concept and a ductless fume hood.
Proper cleaning of reusable medical devices is required for obtaining high-level disinfection and upholding patient safety. When medical devices are not cleaned properly, the results can be costly and, in some cases, deadly. flexible endoscopes were the direct result of improper cleaning procedures (Kenters, 2015). That is nearly half of all HAis related to endoscope use.
A recent press release revealed that in a Georgia VA Medical Center, over four thousand patients had been exposed to improperly reprocessed medical devices. According to the release, it seems staff members had not been properly trained in the reprocessing of medical devices. As a result of a failure to clean and disinfect these devices properly, over four thousand people's health is now in question. Ensuring the best procedures are in place surrounding cleaning and disinfection is vital to the safety and wellbeing of patients.
Human factors drive improper cleaning procedures
The root causes of improper cleaning and disinfection of semi critical devices are numerous and are often unintentional. Many hospitals employ a manual cleaning and disinfection protocol. Manual cleaning and disinfection processes differ depending upon the device being reprocessed, but generally involve soaking devices in large water baths with detergent. Staff use a brush or cloth to physically remove soil and debris from devices, which depending upon the complexity of the device can be a tedious process. Following rinsing, the probes are disinfected, rinsed again, and dried. The devices are then ready to be used for the next procedure.

Often, these steps must be completed sequentially with little to no down-time for staff. These types of manual cleaning processes can be long and arduous, particularly for more complex devices. Further, with the healthcare world increasingly understaffed, the staff tasked with cleaning and disinfecting reusable medical devices often feel under pressure to complete the process as quickly as possible (Andone, 2022). The combination of long complicated protocols, staffing issues, and time constraints leads to missed steps and sub-optimal cleaning and disinfection. One study found that only 1.4% of endoscopes reprocessed using manual cleaning methods and automated disinfection were reprocessed correctly (Ofstead, 2010). Staff must be properly trained in all steps ofthe reprocessing procedure and understand the intricacies of each device to be reprocessed (SGNA, 2018).
Human error is not always to blame when it comes to improperly reprocessed medical devices. Issues with completing the cleaning and disinfection protocols as written may sometimes be harder to pin down. Detergents developed for device cleaning are formulated for use at specific concentrations and temperatures and for specific amounts of time. The use of enzymatic detergents is popular for manual cleaning procedures because of their ability to digest organic material without causing significant damage to the device. However, the enzymes in these detergents can be inactivated over time by certain kinds of soil present on the device or in the detergent solution. Reusing detergents as a way to cut time or save on costs can lower the concentration of active ingredients. In these situations, the detergent will not be as effective and soil or debris may remain on the device, even after cleaning.
The current COVID-19 pandemic has created a perfect storm for HAis linked to medical devices. Hospitals and clinics find themselves extremely short-staffed, with about one-quarter of hospitals reporting critical staffing shortages (Andone, 2022). This means fewer trained staff and even less time to dedicate to each task that must be completed. Devices must be reprocessed quickly and efficiently to give staff time to work on other tasks. Staff working in hospitals report being overworked, exhausted, and burned out, which is known to lead to more mistakes (Hall, 2016).
When mistakes resulting in HAis do occur, infection prevention specialists are generally responsible for investigating the incident and determining a course of action to prevent a similar incident from occurring again. During the COVID-19 pandemic, most infection prevention specialists reported spending more than 75% of their time on COVID-19 related tasks (Percival, 2021). Thus, there has been less time and man power available to investigate potential non-COVID related infections linked to medical devices when they do happen. This makes the need to ensure devices are properly cleaned and disinfected after every use all the more important.
Automation as a solution to improper cleaning
The effectiveness of manual cleaning procedures and the safety of the patients downstream of these processes relies on properly trained staff and sufficient time to complete cleaning protocols. Neither staff nor time are in ample supply, even under the best of circumstances. A simple solution to the problem comes in the form of automated reprocessors.
Automated reprocessors can fill the gap in training and time to ensure devices are cleaned and disinfected correctly every time. Automated reprocessors generally take less time than manual cleaning and disinfection, while giving staff much more downtime during runs to complete other tasks. In this way, automation can reduce workload and time constraints for staff and help alleviate the burden placed on staff members. Because automated reprocessors are significantly less susceptible to mistakes due to frequent workplace distractions and general human error, they also help to mitigate the risk of HAIs.

Utility cart allows for multiple probes to be transported to and from a procedure area.
Together, the efficiency and down-time allowed by automated reprocessors makes them much better suited to assist a busy and short-staffed hospital or clinic. Automated reprocessors generally require much less training than manual procedures and eliminate mistakes related to re-using detergents or disinfectants and issues with temperature, contact time, water sterility, etc.
Lastly, one study showed that automated reprocessors offer more consistent cleaning and disinfection procedures and increase the percentage of endoscopes reprocessed correctly from 1.4% with manual procedures to 75.4% (Ofstead, 2010).
High-level disinfection of semi-critical medical devices is essential to maintaining patient safety, preventing HAis, and reducing healthcare costs. The role of cleaning in the disinfection process cannot be overemphasized. Unfortunately, manual cleaning procedures are often long and difficult procedures that are not well suited to the busy and fast-paced environments of many healthcare facilities. However, automated reprocessors resolve many of the issues of manual procedures by offering efficient and effective cleaning and disinfecting procedures that ensure devices are clean and disinfected each and every time. Automating the cleaning and disinfection steps is one of the simplest ways of promoting efficient hospital procedures and upholding the highest quality of patient care and safety.
References:
Percival 2021: https://www.healio.com/news/infectious-d isease/20210514/pand emic-strains-resou
rces-for-hai-prevention-and-surveillance Ofstead, 2010:
https://pubmed.ncbi.nlm.nih.gov/20679783/
Andone, 2022: https://www.cnn.com/2022/01/09/health/us-coronavirus-sunday/index.html
SG NA, 2018: https://www.sgna.org/Portals/0/SG NA%20Standards%20of%20infection%20prevention%20i
n%20reprocessi ng_FINAL. pdf?ver=2018- l1-16-084835-387
Alfa, 2009: https://link.springer.com/article/10.1186/1471-2334-9-56#Secl 6
Roberts, 2013: https://www.ajicjournal.org/article/50196-6553(13)00018-7/fulltext
CDC, 2008: https://www.cdc.gov/infectioncontrol/pdf/guidelines/disinfection-guidelines-H.pdf
Lewis, 1995: https://www-natu re-com.Iibproxy.Iib.unc.edu/articles/nm0995-956.pdf
Lambert, 2001: https://sfamjournals.onlinelibrary.wiley.com/doi/pdf/10.1046/j.l
365-2672.2001.01422.x Rutala, 1997:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172936/pdf/100597.pdf
Rutala, 2014: https://jamanetwork.com/journals/jama/fullarticle/1911309#jed140082r8
Donlan, 2002: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2732559/
Hall, 2016: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4938539/
Kenters, 2015: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4554517/
Checklist for Reprocessing TEE Ultrasound Probes with Automation
This checklist is provided as an outline of steps required to successfully reprocess a TEE ultrasound probe with the incorporation of automation. These steps are intended to follow guidelines and recommendations from manufacturers of the ultrasound probe, high-level disinfectants and recognized governmental and professional bodies. This checklist should be used as a reference for individual healthcare infection control professionals. ALWAYS DON PROPER PPE!
Step 1: Point of Care - Bedside
At patient bedside, immediately after removal from patient, apply an enzyme to the probe shaft with either a cloth or other applicator to remove organic and inorganic matter. By performing this step, it aids in preventing drying of the gross material on the probe shaft which can lead to biofilm formation.
Step 2: Transporting to Clean and Disinfect
Transport the TEE probe to the area designated for performance of the manufacturer's directed enzymatic cleaning and high-level disinfection steps. Caution should be taken to minimize exposure to the potential biological hazard of the dirty TEE probe as well as to protect the probe from damage. Consult probe manufacturer's IFU for handling and care.
Step 3: Electrical Leakage Testing
Perform electrical leakage testing per probe manufacturer's guidelines. Each TEE probe has different measurements, so consult your probe manufacturer's IFU. Follow the IFU from the disinfector manufacturer to complete the necessary steps for electrical leakage testing.
Step 4: Cleaning and High-level disinfection of TEE ultrasound probe
Once the TEE Probe has been placed into the automated cleaner disinfector, follow the screen prompts to perform cleaning and high-level disinfection and rinse of the TEE ultrasound probe. The device will have the operator enter into the microprocessor the following data: operator name or designation, probe name or designation, and chemical lot number. With single-use chemistry, the expiration date on the bottle should be observed and if the expiry date has occurred, the chemical should not be used. NO MRC test strip is required to validate the efficacy of the disinfectant as long as it is used within the shelf life as cleared by the manufacturer with the FDA.
Step 5: Drying of probe after removal from cleaner disinfector
Once the final rinse is complete, remove the probe from the device. Apply a drying cloth, single-use, lint-and contaminant-free, to the shaft as you remove the probe from the machine. Care should be observed not to hit or bang the distal tip of the TEE probe as this portion is the most delicate.
Step 6: TEE probe storage
Place the high-level disinfected and dried TEE probe into a storage cabinet designed to hang the handle, electrical connector and shaft vertically and freely. Make sure that the handle, cable and electrical connector remain separate from the insertion shaft. All portions of the TEE, other than the insertion shaft, have only been surface disinfected while the insertion shaft has been high-level disinfected. Attention should be given not to bang or hit the distal tip of the probe as this portion is the most delicate. Per TJC requirements, the storage cabinet should allow the probes to hang vertically and have HEPA filtered air bathe them during storage.
Step 7: TEE probe transport
Remove the probe from the storage cabinet and transport the TEE probe to the procedure room in a manner that ensures the probe the following conditions: 1) Secure as to not drop or bang the probe in transit, 2) Within an enclosure designed not to allow cross-contaminants to be reintroduced onto the probe, 3) Enclosure designed to transport the probe without damaging due to over coiling or components hitting each other during transit.